Scientists Supercharge HPV Cancer Vaccine With a Tiny Structural Shift
A Tiny Structural Shift Supercharged the HPV Cancer Vaccine Into a Tumor-Fighting Powerhouse
For more than a decade, researchers at Northwestern University have been quietly uncovering one of the most transformative lessons in vaccine science: it’s not just what a vaccine contains that matters—it’s how those ingredients are arranged.
In a breakthrough that could reshape the future of cancer immunotherapy, scientists have demonstrated that a minute structural tweak to an HPV cancer vaccine transformed it from a modest immune stimulator into a powerful tumor-destroying agent. The discovery, published in a recent study, reveals how the precise spatial organization of vaccine components can dramatically enhance the body’s ability to recognize and attack cancer cells.
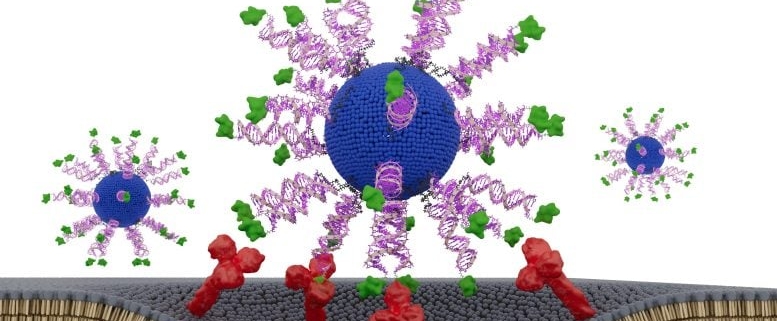
The research centers on a class of molecules known as spherical nucleic acids, or SNAs. These are nanostructures where genetic material—such as DNA or RNA—is arranged in a dense, spherical configuration around a nanoparticle core. Unlike traditional linear nucleic acids, SNAs present their genetic payload in a three-dimensional, radially organized pattern that the immune system processes in a fundamentally different way.
In the case of the HPV cancer vaccine, the team took an existing antigen—a protein fragment derived from the human papillomavirus that is known to trigger immune responses—and reconfigured it into an SNA format. This seemingly small change had outsized effects. The SNA-based vaccine not only elicited stronger immune responses but also trained the immune system to more effectively target and eliminate HPV-infected or HPV-associated cancer cells.
What makes this discovery particularly compelling is the breadth of evidence supporting it. Over the past 10 years, the Northwestern team has tested this principle across multiple vaccine platforms and disease targets. Time and again, they found that the spatial arrangement of antigens—whether in cancer, infectious disease, or autoimmune contexts—could be as decisive as the antigen itself.
The implications are profound. Traditional vaccine design often focuses on identifying the right antigen or adjuvant—the immune-stimulating ingredient. But this work suggests that the architecture of the vaccine, the way its components are physically organized at the nanoscale, can be just as critical. It’s a paradigm shift that could lead to more effective vaccines not only for HPV-related cancers but potentially for a wide range of malignancies and infectious diseases.
HPV, or human papillomavirus, is a leading cause of cervical cancer and is also associated with cancers of the throat, anus, and other regions. While preventive HPV vaccines like Gardasil have been game-changers in reducing infection rates, therapeutic vaccines that can treat existing HPV-related cancers have proven more elusive. The Northwestern team’s SNA-based approach offers a promising new avenue, potentially bridging the gap between prevention and treatment.
The mechanism behind the enhanced efficacy appears to be rooted in how SNAs interact with immune cells. Their unique structure allows them to be taken up more efficiently by certain immune cells, particularly those involved in initiating and sustaining anti-tumor responses. Once inside, the SNA-delivered antigens are processed and presented in a way that maximizes immune activation, leading to a more robust and durable defense against cancer cells.
This isn’t just a laboratory curiosity. The researchers have already begun translating their findings into clinical applications, with plans to advance SNA-based vaccines into human trials. If successful, this could mark the beginning of a new era in cancer immunotherapy—one where the geometry of a vaccine is as important as its genetic content.
The broader scientific community has taken note. Experts in immunology and nanotechnology are hailing the work as a prime example of how interdisciplinary approaches—combining insights from chemistry, biology, and materials science—can yield unexpected and transformative breakthroughs. It also underscores the importance of continued investment in basic research, where seemingly esoteric questions about molecular arrangement can lead to real-world medical advances.
As the field moves forward, the Northwestern team’s findings serve as both a scientific milestone and a call to action. They remind us that in the fight against cancer, sometimes the smallest changes—down to the arrangement of atoms—can make the biggest difference.
Tags, viral words and phrases:
HPV cancer vaccine breakthrough
Spherical nucleic acids (SNA) revolutionize immunotherapy
Tiny structural tweak supercharges tumor-fighting power
Northwestern University cancer vaccine discovery
Nanoparticle vaccine architecture matters
HPV-associated cancers targeted with new vaccine design
Immune system supercharged by SNA technology
Next-generation cancer vaccines on the horizon
Vaccine geometry as important as genetic content
Therapeutic HPV vaccine advances
Cancer immunotherapy paradigm shift
SNAs enhance immune response to antigens
HPV vaccine moves from prevention to treatment
Nanotechnology meets cancer biology
Small change, big impact in vaccine science
Tumor-destroying vaccine breakthrough
HPV cervical cancer therapeutic advances
Immune cells activated by SNA vaccines
Future of cancer treatment redefined
Vaccine design reimagined at the nanoscale,



Leave a Reply
Want to join the discussion?Feel free to contribute!